Understanding ACEs:
ACEs are risk factors for poor mental and physical health. They also increase the likelihood of individuals engaging in risky life style decisions with poor health outcomes later in life. Although ACEs are experienced during childhood, the biologic changes they may cause can last a lifetime.
In fact, as adults, children who have experienced four or more ACEs are:1,2,3
| Over 1.5x more likely to have diabetes. | |||||
| 2x more likely to suffer from ischemic heart disease. | |||||
| 2x more likely to have cancer. | |||||
| Almost 2.4x more likely to have a stroke. | |||||
| 4x more likely to have chronic bronchitis/emphysema. | |||||
| 2-5x more at risk of attempted suicide compared to individuals who did not experience ACEs. | |||||
| 5x more likely to have an increased risk for depressive disorders. | |||||
| Over 1.5x more likely to have diabetes. | |
| 2x more likely to suffer from ischemic heart disease. | |
| 2x more likely to have cancer. | |
| Almost 2.4x more likely to have a stroke. | |
| 4x more likely to have chronic bronchitis/emphysema. | |
| 2-5x more at risk of attempted suicide compared to individuals who did not experience ACEs. | |
| 5x more likely to have an increased risk for depressive disorders. |
Our patients need to understand that ACEs do not determine one’s destiny – but are dose-dependent risk factors. Reducing the number of ACEs experienced during childhood will decrease this risk. With directed screening, referral, and support, we can minimize the health effects of ACEs.4
Incorporating the science of ACEs in practice:
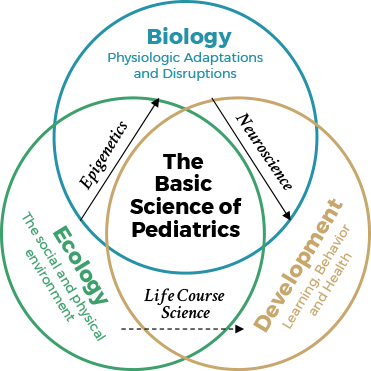
The American Academy of Pediatrics endorses the ecobiodevelopmental model of Pediatrics (see image), and recommends that we address the social determinants of health, including ACEs, with our patients and families. We can examine these factors through screening and identifying our patient’s exposure to adverse experiences, and taking steps to reduce this risk. We can also discuss with families the importance of providing a safe, stable and nurturing home and environment for their children.
Before screening, make yourself aware of the supportive resources that may be available to families.
The ACE score
- The Kaiser Permanente ACE survey has 10 questions. The score is a sum of the positive responses.
- Before incorporating the ACE survey into patient care, determine how your practice will use the information.
Download the ACEs Questionnaire
Click here to download the ACEs questionnaire
Download the Childhood Trust Events Survey and Caregiver Form to find an adolescent ACE score as additional tools to open a dialogue between the provider and family
Other screening tools
How an ACEs score helps in practice
Parent’s ACE score in pediatric practice:
- Strengthens the doctor/parent relationship.
- Educates the parent about ACEs.
- Supports discussions of parent self-care that promote child resilience.
- Offers a non-judgmental opportunity to recommend changes to the child’s environment that will reduce the child’s ACE exposure and build their social-emotional health.
- HELPFUL TIP: Some providers find it will be easier and just as useful to ask for a total of score of ACEs rather than asking which specific ACEs a parent experienced.

Child screening in pediatric practice:
- The ACE survey can identify risk, engage parents and guide future healthcare.
- Social Determinants of Health screening can identify specific interventions to reduce ACEs and build resilience. SEEK (Safe Environment for Every Kid) is one such example.
- Social and Emotional Health screening will help to identify children who are failing to meet developmental milestones and who should be referred for interventions.
- Strengthens the doctor/parent relationship.
- Educates the parent about ACEs.
- Supports discussions of parent self-care that promote child resilience.
- Offers a non-judgmental opportunity to recommend changes to the child’s environment that will reduce the child’s ACE exposure and build their social-emotional health.
- HELPFUL TIP: Some providers find it will be easier and just as useful to ask for a total of score of ACEs rather than asking which specific ACEs a parent experienced.
- The ACE survey can identify risk, engage parents and guide future healthcare.
- Social Determinants of Health screening can identify specific interventions to reduce ACEs and build resilience. SEEK (Safe Environment for Every Kid) is one such example.
- Social and Emotional Health screening will help to identify children who are failing to meet developmental milestones and who should be referred for interventions.
Exposure to ACEs disguised as medical conditions
Children who have experienced ACEs can have behavioral health symptoms that mimic other conditions such as ADHD, ODD, conduct disorder, bipolar disorder, or anger management difficulties.3 Children can also have eating, sleeping or digestive issues. Consider ACEs in the differential diagnosis and refer to trauma specific interventions when present.4
You can find more information on specific interventions by visiting our resource library here.
You’ve identified that a child may have experienced ACEs. Now what?
Promote childhood resilience by helping parents create a safe, stable, nurturing environment. Childhood resilience will alter how ACEs are experienced, reduce or prevent toxic stress, and lessen or eliminate negative outcomes from ACEs.5
- Parental ACEs may affect the subsequent generation.6
- Encourage discipline rather than punishment and offer guidance for challenging behaviors.
- Recommend healthy family interactions like eating together, reading, and the importance of routines.
- Promote the parent’s self-care to set a positive example.
- Meditation, exercise, healthy eating, a full night’s sleep.7
ACEs are dose-dependent, so reducing their exposure is critical. As a healthcare professional, you can connect families to resources within the community and can help:
- Share a resource list with families to assist with food insecurity, unsafe housing, and economic hardship.
- Connect parents who may be suffering from a mental illness with the appropriate mental health professional.
- Promote safety when family violence exists and report child abuse and neglect.
Make your practice “ACEs Informed”
- Educate your entire staff about ACEs, toxic stress, and resilience.
- Help them to identify high-risk patients/families through screening.
- Practice how to discuss ACEs, toxic stress and resilience with your patients (and their parents, if applicable).
- Develop quick & useful responses to positive screens.
Taking action to further our understanding.
We’re still learning more about ACEs, their effects, and ways to combat them. It’s up to us in the medical community to improve identification and implement effective interventions to drive better outcomes in the future. But we all need to work together.
Measure outcomes
- Record results of screening tests and measures.
- Describe and count types of interventions prescribed.
- Measure both the parent and patient satisfaction.
- ConductPDSA (Plan-Do-Study-Act) cycles of improvement efforts.
- Share your successes, challenges, and failures with Joining Forces for Children and other organizations. This is a learning process to find the most effective intervention and tactics for your patient population.
We’re in this together.
Local and national resources are eager to help you and your organization become better prepared to help children who are experiencing ACEs and toxic stress.
- Connect with Joining Forces for Children to learn about other local organizations and resources.
- Or nationally, join ACEs Connection: A community-of-practice social network (http://www.acesconnection.com/).
Need a question answered?
Or for additional resources:
1. Felitti, V.J., Anda, R.F., Nordenberg, D., Williamson, D.F., Spitz, A.M., Edwards, V., & Koss, M. P. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245-258.
2. Chapman, D.P., Whitfield, C.L., Felitti, V.J., Dube, S.R., Edwards, V.J., & Anda, R.F. (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82, 217–225.
3. Dube, S.R., Felitti, V.J., Anda, R.F., Chapman, D.P., Williamson, D.F., & Giles, W.H. (2001). Childhood Abuse, Household Dysfunction, and the Risk of Attempted Suicide Throughout the Life Span Findings From the Adverse Childhood Experiences Study. JAMA, 286(24), 3089-96.
4. Kerker, B.D., Zhang, J., Nadeem, E., Stein, R.E.K., Hurlburt, M.S., Heneghan A., Landsverk, J., & Horwitz, S.M. (2015) Adverse Childhood Experiences and Mental Health, Chronic Medical Conditions, and Development in Young Children. Academic Pediatrics, 15(5), 510-517.
5. American Academy of Pediatrics. (2017). Helping Foster and Adoptive Families Cope with Trauma: A Guide for Pediatricians. Healthy Foster Care America. Retrieved from https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/healthy-foster-care-america/Pages/Trauma-Guide.aspx#trauma
6. The National Child Traumatic Stress Network. “National Child Traumatic Stress Network Empirically Supported Treatments and Promising Practices.” http://www.nctsn.org/resources/topics/treatments-that-work/promising-practices#q4
7. Konnikova, Maria. “How People Learn to Become Resilient.” The New Yorker. February 11, 2016. http://www.newyorker.com/science/maria-konnikova/the-secret-formula-for-resilience
8. American Academy of Pediatrics. “Adverse Childhood Experiences and the Lifelong Consequences of Trauma.” 2014.
9. Zero to Three. “Creating Routines for Love and Learning.” February 20, 2010. Retrieved from https://www.zerotothree.org/resources/223-creating-routines-for-love-and-learning
